Despite the recent disappointing news about two fundamental programs seeking Huntington’s disease treatments, significant drug-discovery initiatives proceed steadily. They include two major clinical trials: KINECT-HD, sponsored by Neurocrine Biosciences, and PROOF-HD, backed by Prilenia Therapeutics.
As reported in Part I of this two-part series and a previous article, Roche announced that it had halted dosing in its historic Phase 3 gene silencing clinical trial, followed by Wave Life Sciences’ revelation that a similar effort to reduce the level of mutant huntingtin protein had fallen short.
In all likelihood, these drug candidates – at least the current version of them – will not become HD treatments.
However, other candidates abound.
“Our pipeline is full of hope,” said George Yohrling, Ph.D., the
chief scientific officer for the Huntington’s Disease Society of America (HDSA), in a March 25 webinar
held to address the devastating clinical trial news. “Our pipeline is deep and
diverse.”
The HD research community “has not put all their eggs” in the Roche “basket,” Dr. Yohrling explained. “We know what causes the disease, and it’s the expansion of the huntingtin gene and the expression of this mutant protein. There is a wide array of approaches that we are using to tackle that. We’re hopeful that one or many of them will prove efficacious and modify the course of the disease.”
Advancing programs
Although two Wave drug compounds failed in early-stage trials, the company plans to start a trial of a third compound later this year.
Both Roche and Wave are scheduled to make the first scientific presentations about their recent results this week at the greatly anticipated 16th Annual HD Therapeutics Conference, April 27-29, a virtual event because of the COVID-19 pandemic. The research community is confident that a deep analysis of these studies will guide its next steps in the quest for therapies.
Researchers and companies are investigating dozens of distinct designs for the type of drug used by Roche and Wave, an antisense oligonucleotide (ASO).
Using surgery to inject its drug directly into the brain, Uniqure has started the first-ever HD gene therapy safety trial in a small number of trial participants.
Triplet Therapeutics aims to start a Phase 1 clinical trial in the second half of this year of a unique ASO targeted at stopping the mutant huntingtin gene’s tendency for continued expansion with age (click here to read more).
Genetic modification is not the only approach under study,
however. Several other firms have Phase 2 programs in the works to treat
symptoms and reduce disability due to HD,
and Neurocrine expects to complete KINECT-HD – its Phase 3 trial of
a chorea-reducing drug called valbenazine – by year’s end. Chorea is the
involuntary movements that afflict many people with HD. (On KINECT-HD, also click here.)
Two similar drugs for chorea – Xenazine and Austedo – are the only HD drugs approved by the U.S. Food and Drug Administration (FDA). They do not stop progression of the disease.
A big goal: helping HD people function normally
A second major study, called PROOF-HD, is currently underway, led by the Huntington Study Group (HSG), and sponsored by Prilenia. This is a Phase 3 trial (the final step before a drug can be approved by the FDA) of a drug called pridopidine, which is proposed to improve function in people in the early stages of HD.
PROOF-HD stands for “PRidopidine Outcome On Function In Huntington Disease.”
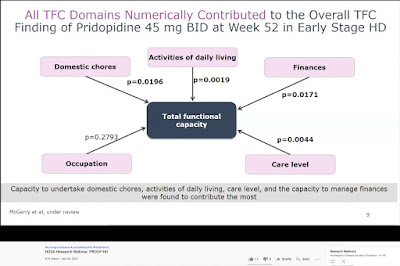
The clinical trial investigators believe that, if tested successfully, pridopidine would help early-stage HD-afflicted individuals maintain the ability to function normally in five key areas: occupation/employment, managing personal finances, performing household chores, performing activities of daily life (such as bathing and dressing), and the ability to live in a home environment. These five domains comprise the Shoulson-Fahn Total Functional Capacity Scale (TFC), developed almost 40 years ago, and used daily in HD clinics and research studies since then.
“The bigger the effect, the better,” Prilenia CEO Michael Hayden, M.D., Ph.D., said in an April 1 interview about pridopidine with Evaluate Vantage. “But any significant change in TFC would be regarded as meaningful. There’s never been a drug that has had any impact on TFC.”
Dr. Hayden is one of the world’s foremost HD scientists (click here to watch our 2011 interview at the Therapeutics Conference.) Prior to founding Prilenia in 2018, Dr. Hayden served as the president of global R&D and chief scientific officer at Teva Pharmaceutical Industries, Ltd. from 2012-2017, where he oversaw ongoing research on pridopidine. He is also a professor at the University of British Columbia and a senior scientist at the Centre for Molecular Medicine and Therapeutics, having mentored over 100 graduate students.
In a January 28 HDSA webinar, Sandra Kostyk, M.D., Ph.D., a professor Ohio State University and the co-principal investigator for PROOF-HD in the U.S., pointed out that individuals’ Total Functional Capacity ranges from zero (severely reduced function) to 13 (full function). In early and mid-early HD, people on average lose about one point on the scale a year, she explained.
In later stages of the disease, TFC may be less reflective of the rate of decline, Dr. Kostyk continued.
A slide from the January 2021 HDSA webinar on the PROOF-HD trial illustrating the Total Functional Capacity Scale and the effect of pridopidine (screenshot by Gene Veritas, aka Kenneth P. Serbin)
Stopping the house from burning down
As an HD gene carrier who saw his mother devastated by the disease, I have most feared losing my ability to function normally.
In three previous clinical trials of pridopidine, carried out between 2008 and 2018, both the original developer of the drug and Teva failed to achieve the goal of reducing HD persons’ difficulties with both voluntary and involuntary movements. At that time, scientists thought that pridopidine affected levels of dopamine, an important chemical in the brain affecting movements in both HD and Parkinson’s disease.
However, additional analysis (done after the trials) showed that patients taking the study drug showed a slower decline in TFC than expected from previous studies. “In early patients with Huntington disease we have shown that the functional capacity may be maintained,” Dr. Hayden observed in a January HSG podcast. “There also appears to be an improvement and less deterioration in patients with early HD.”
Referring
to research conclusions published in the Journal of Huntington’s Disease
last December and co-authored by Dr. Hayden and five others, he asserted that the stabilized
TFC results were the “first time that this has ever been shown in any analysis
for any drug. This was exciting.” Significantly, the FDA accepts TFC
as a way of measuring drug efficacy in HD clinical trials, he added.
Those observations now require confirmation in PROOF-HD, Dr. Hayden said.
Also, he continued, pridopidine “appears to have beneficial effects around protecting neurons,” whatever the injury might be. The goal, he said, is to prevent these brain cells from dying – one of the major symptoms of HD.
“You want to treat them before they've died,” he explained. “If you're trying to stop a fire taking care of a house, you don't want the house to be burned down. And that's why treating early becomes effective because there are still injured neurons, but not dead neurons.”
In the HDSA webinar, Dr. Kostyk referred to pridopidine as a possible “disease-modifying intervention – something that slows the course of the disease.” The data indicate that early-stage HD patients could obtain “long-term beneficial effects” from an approved pridopidine drug for five years or more, she said.
That could buy valuable time for older asymptomatic individuals like me and the HD community in general as we await other gene-modifying or huntingtin-lowering drugs.
Prilenia: seeking to soothe the impact of disease
Dr. Hayden explained the name and goals of Prilenia: “Prilenia, which comes from pri, as in pridopidine, and lenia, which comes from the Greek, to sooth or to cure. It's an aspiration that we can have some impact on soothing some aspects of this disease and potentially others as well.”
Privately held and based in Israel and the Netherlands, in 2020 Prilenia raised $68.5 million to support PROOF-HD and also a Phase 2/3 trial in sufferers of amytrophic lateral sclerosis (ALS).
The ALS trial is currently enrolling participants at 54 sites across the US.
Pridopidine taken as a pill
For HD sufferers, Pridopidine has another major advantage: whereas ASOs so far have been injected into the spine and Uniqure’s drug has been infused via brain surgery, pridopidine in the PROOF-HD trial is very conveniently dosed in a 45-milligram pill – a hard gelatin capsule – taken twice daily (click here for official details of the trial).
Pridopidine has been extensively studied in several previous clinical trials over more than a decade, with more than 1,300 people taking the drug, most of them with Huntington’s, Dr. Kostyk said. As a result, researchers have high confidence in its safety, she added.
Other HD research projects and biopharmaceutical firms are seeking so-called small molecule drugs that can enter cells easily and be taken as a pill.
A key receptor in the brain
Dr. Hayden and his colleagues now believe that the benefits of pridopine are due to its ability to activate the sigma-1 receptor (S1R). “It’s highly selective and fairly potent,” Dr. Hayden explained about the action of pridopidine on S1R in response to a question that I posed about the drug’s basic mechanism during his presentation at the 27th Annual HSG Meeting (held online) in October 2020.
Dr. Hayden observed further that ample data demonstrates that activation of S1R leads to protection of neurons. Deficiencies in S1Rs leads to disease. He cited the case of patients lacking the S1R gene, resulting in juvenile onset ALS.
“The activation of the sigma-1 receptor has multiple mechanisms of action that should lead to neuroprotection in HD and help stabilize cell function,” stated Dr. Kostyk, noting that S1Rs are plentiful in the striatum – the inner core of the brain where HD is especially devastating – and in the cortex, the large outer area of the brain in charge of thought, language, and consciousness.
“One could think of the role of S1R as being like that of a high school guidance counselor,” Martha Nance, M.D., director of the HDSA Center of Excellence at Hennepin HealthCare in Minneapolis, MN, wrote me in an e-mail. “When the receptor is turned on, materials, molecules, and traffic within the cell flow as it should, and the cell stays healthy, much as the counselor helps students in trouble to be safe, find resources to keep healthy, and stay in school. Supporting S1R early in the course of HD might help more brain cells to remain healthy and function well for longer.”
A relatively easy trial seeking practical results
Initiated last October, PROOF-HD investigators hope to enroll a total of 480 clinical trial volunteers by year’s end at 30 sites in the U.S. and Canada and 30 more in Europe. Over 15 months, half will get pridopidine, and half will get a placebo. Patients must have a diagnosis of HD, be 25 or older (no upper age limit), and have a TFC score of at least 7, in line with the project’s goal of testing the drug in the earlier stages of the disease.
Participants will undergo measurements of their TFC, cognition, quality of life, and motor symptoms (difficulties with voluntary and involuntary movements). They will also get blood and safety tests. All participants can take part in the potential extension of the trial, with everybody receiving the drug. Dr. Kostyk described PROOF-HD as an “easy” trial, with no brain scans or spinal taps (used in the Roche trial, for instance). The study design has been adapted to accommodate the challenges posed by COVID-19.
PROOF-HD emphasizes practical results. “What’s most important for us it to get an agent out that’s working,” Dr. Kostyk said, and “not necessarily” the kinds of measurements used in other trials in order to demonstrate how the drug works.
A separate trial might be designed later for later-stage HD-afflicted individuals, Dr. Hayden said.
For more information on PROOF-HD, click here or call 800-487-7671.
A potential major step forward
“Our overall goal is to get this agent FDA-approved as soon as possible so that we can start using it in individuals affected by Huntington’s disease,” said Dr. Kostyk. The more quickly patients enroll in the study, the sooner it will be completed, hopefully by late 2022 or early 2023. Because this is a Phase 3 trial, if it is successful, the next step will be an application to the FDA for approval as a drug that doctors can prescribe.
Andrew Feigin, M.D., the HSG chair and principal investigator in the U.S. for PROOF-HD, said in the HDSA webinar that Prilenia has also shown interest in a possible future trial involving pre-symptomatic individuals like me.
Past skepticism about pridopidine focused on the lack of hard evidence that the drug could really slow HD progression (click here to read more). However, that debate came before the discovery of a clearer picture of pridopidine as a potential protector of neurons.
As will all clinical trials, the Huntington's community will be rooting for success in PROOF-HD. Although pridopidine may not cure HD, enabling people to have a few more years of normal daily function would be a major step in the quest to manage this complex disease.
No comments:
Post a Comment