Progress towards effective treatments for Huntington’s disease relies on the affected families’ collaboration with researchers exploring the frontiers of science.
The potentially pathbreaking findings featured at the recently completed 19th Annual HD Therapeutics Conference, sponsored by the nonprofit CHDI Foundation, Inc., led CHDI Chief Scientific Officer Robert Pacifici, Ph.D., to declare that the community will achieve therapies.
In this article I highlight the scientists’ work with a photo essay on their conference presentations and some of their key observations.
I cover most of the presentations. For detailed reports on the conference, see the articles in HDBuzz by clicking here, here, and here. Later CHDI will post videos of the presentations on its website. It is also preparing a video “postcard” of the event.
In
recent decades, Huntington’s breakthroughs have resulted from the increasing
amount of human data, which Dr. Pacifici and other scientists say is the best
way to study the disease and develop potential therapies. The presentations at
this conference especially reflected this trend. Researchers such as Matthew
Baffuto, B.S., of the Heintz Lab at The Rockefeller University (in the photo above),
recognized the importance of postmortem donations of HD-affected individuals’
brains and other human samples for their research. Baffuto’s final slide
included a dedication: “To the HD patients and families who make this human
research possible and for whom we continue to strive for a cure.” (All photos by Gene Veritas, aka Kenneth P. Serbin) (Click on an image to make it larger.)
The first wave of attempts by pharmaceutical companies to defeat Huntington’s has involved attempts to lower the amount of the abnormal huntingtin protein (HTT) in patients’ brains. In many of these approaches, this also means lowering the amount of normal HTT. The lab of Jeff Carroll, Ph.D., a scientist at the University of Washington and a HD gene expansion carrier like me, has extensively studied huntingtin lowering in mice. Normal huntingtin is necessary for adult mice to function, Dr. Carroll observed. Huntingtin lowering is not a “bad idea, just that there’s a floor between 50 percent and zero percent HTT,” he said.
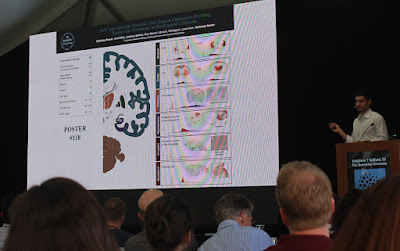
Tony Reiner, Ph.D., of the University of Tennessee Health Science Center, presented the latest findings of his work comparing HD mouse brains to human tissue from deceased HD-affected individuals. He also focuses on how HD affects the various regions of the brain differently. This photo illustrates how Dr. Reiner uses antibodies to measure the complications that arise in HD mouse brains.
Sarah Tabrizi, M.D., Ph.D., of University College London, discussed her lab’s research on somatic expansion, the tendency of the abnormal huntingtin gene to expand with time and become more harmful to the brain. She presented data on developing drugs to interact with modifier genes, which can impact somatic expansion and therefore the age of disease onset. Dr. Tabrizi focused on the modifier gene MSH3 as an ideal therapeutic target. For this research, the Tabrizi lab has utilized stem cells, CRISPR gene editing techniques, and antisense oligonucleotides, used in huntingtin lowering drug programs and other HD research projects.
Ricardo Mouro Pinto, Ph.D., of Harvard University Medical School, presented his lab’s work on genetic modifiers of somatic expansion. Dr. Pinto has implicated the so-called DNA mismatch repair pathway as a critical driver of somatic expansion. His lab is also developing CRISPR-based strategies as potential therapies. Dr. Pinto’s team was recently awarded a grant from the Hereditary Disease Foundation to continue the search for therapies.
Mark D. Bevan, Ph.D., of Northwestern University, spoke on his lab’s latest findings in HD mice, in particular the dysregulation and rescue of subthalamic nucleus, involved in the suppression of movement. Dr. Bevan highlighted the need for both huntingin-lowering and somatic expansion therapies to have widespread delivery into the brain.
Osama Al-Dalahmah, M.D., Ph.D., of the Columbia University Irving Medical Center, discussed the major role of astrocytes in HD. There are over 100 different brain cell types. Astrocytes are cells that provide physical and chemical support to other cells such as neurons, key in the brain. As a neuropathologist, Dr. Al-Dalahmah analyzes post-mortem brain tissues. Among other observations, he noted that astrocytes can be neuroprotective. His lab is working on ways to protect neurons in HD.
Scientist Baffuto’s wide-ranging presentation focused on specifying cell types in unraveling both the molecular mechanisms underlying somatic expansion and also the path of the disease. The Rockefeller team developed what it describes as an “innovative methodology” for deep profiling of cellular processes in the brain. The technique is fluorescence-activated nuclear sorting (FANS). As shown in one of Baffuto’s slides, they used FANS to detail the disease process in key areas of postmortem HD-afflicted brains: the striatum, cortex, thalamus, hippocampus, amygdala, and cerebellum.
Scientists continue to debate exactly what triggers Huntington’s. Assessing the impact of somatic expansion, the Harvard University Medical School team studying HD proposed a new model for how somatic expansion contributes to HD pathology. Bob Handsaker, B.S., explained that, until recently, scientists thought that the DNA triplet repeat creates a toxic protein whenever the CAG repeat length is greater than 40 and that HD pathology arises from lifelong exposure to this toxic protein, similar to how smoking damages the lungs. (The abnormally repeated DNA word CAG is the genetic root of HD.)
New research has
challenged this idea in three important ways: First, there is much more somatic
expansion than had been appreciated, with affected neurons expanding to reach
over 400 CAG repeats. Second, this somatic repeat expansion starts slowly and
then accelerates over time, like a "slowly ticking DNA clock” in each
individual neuron. Third, the evidence suggests that modest somatic expansion,
up to a repeat length of 150 CAGs, does not create a protein that is toxic -
the toxic effect in each individual neuron only begins above this longer
repeat-length threshold. Along with other research presented, this finding
underscored that there may be a longer window of opportunity than had
previously been appreciated for any therapeutic interventions that act to slow
or block somatic expansion. This is because in the first few decades of life in
a person with HD, the DNA in most neurons has typically not expanded to reach
this toxic threshold.
Darren G. Monckton, Ph.D., of the University of Glasgow, presented his new research on biomarkers, signs of a disease and indicators of whether a drug has efficacy. Dr. Monckton focused on biomarkers in areas of the body outside the brain such as blood, in particular regarding the degree of somatic expansion and measuring it over time.
Carlos Bustamente, Ph.D., a Venezuelan American geneticist and the founder and CEO of Galatea Bio, Inc., advocated for enabling precision medicine around the globe. Dr. Bustamante observed that new technological advances have made it faster and less expensive to understand human genomes but most of such resources have gone to understanding predominantly northern European communities. He pointed out the need to expand the genetic dataset to other parts of the globe. Dr. Bustamante also explained how genetic differences in the global population have contributed to differences in the geographic prevalence of Huntington's.
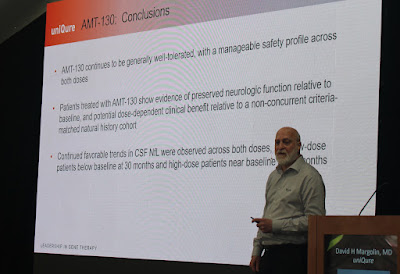
David Margolin, M.D., Ph.D., the vice president for clinical development at uniQure, presented an update on the early-stage (Phase 1/2) clinical trial of the company’s gene therapy drug, AMT-130, involving 39 trial volunteers in the U.S. and Europe. Dr. Margolin reported that, relative to baseline, volunteers treated with AMT-130 showed evidence of preserved neurological function. So far, the drug has proved to be safe.
Amy-Lee Bredlau, M.D., the senior medical director at PTC Therapeutics, presented interim safety and biomarker data for the company’s huntingtin-lowering pill, PTC-518, in PIVOT-HD, a Phase 2 trial. At this stage, the drug has been shown to be safe and has achieved a lowering of huntingtin in the blood – although data do not yet show whether the lowering is also occurring in the brain.
From left to right, Roche researchers Jonas Dorn, Ph.D., Peter McColgan, M.D., Ph.D., and Marcelo Boareto, Ph.D., reanalyzed the data from the firm’s first attempt at a Phase 3 huntingtin-lowering trial program, which in 2021 ended without the drug tominersen showing the necessary efficacy for approval as a drug. The scientists discussed ways to improve clinical trial design, including for GENERATION HD2, a less ambitious, Phase 2 trial of tominersen in a smaller number of volunteers. GENERATION HD2 is in progress.











No comments:
Post a Comment