At the recent 20th Huntington’s Disease Therapeutics Conference in February, four pharmaceutical companies provided updates on their key clinical trial programs, demonstrating that they had overcome basic safety hurdles and revealing plans to have their drugs potentially approved as therapies (treatments) for delaying the progression of HD symptoms.
All four programs use drugs to lower the amount of harmful mutant huntingtin protein in the brain cells of patients.
In the first of two articles on these programs, I described the projects of PTC Therapeutics and Roche.
In this article, I cover the presentations made by Wave Life Sciences and uniQure.
These updates took place during the conference’s first session on February 25, the first day of the three-day event.
In a post-conference interview Robert Pacifici, Ph.D., the chief scientific officer for CHDI Foundation, Inc., the conference sponsor, told me that that there is “great promise” regarding these four programs’ potential HD therapies.
Attacking only the bad protein, preserving the good one
Jane Atkins, Ph.D., Wave’s senior vice president for portfolio strategy and program management, provided an update on the company’s groundbreaking program.
Like Roche’s tominersen, Wave’s WVE-003 is an antisense oligonucleotide, an artificial strand of DNA that blocks or lowers the production of the huntingtin protein.
However, whereas tominersen and PTC’s votoplam (a splicing modulator) reduce both the mutant and normal huntingtin protein, Wave’s drug is uniquely allele-selective: it attacks just the bad protein and allows the good one to carry out its essential actions unhampered.
Clinical trials for drugs usually go through three phases. If the last is successful, the drug can receive approval from the U.S. Food and Drug Administration (FDA).
In 2021, in small clinical trials, precursors WVE-120101 and WVE-120102 failed to reduce the bad protein. Wave then developed WVE-003, which entered a clinical trial that same year.
At the conference, Dr. Atkins reported that in June 2024 the Phase 1b/2a SELECT-HD study of WVE-003 produced positive results, “including the first allele-selective silencing in any disease.”
“A growing body of literature” supports the importance of the good huntingtin protein, she explained, as it sustains the health of brain cells.
Slowing the shrinking of the brain
In the clinical trial, the bad protein was reduced as much as 46 percent in some volunteers, exceeding the overall goal of 30 percent, Dr. Atkins said, noting that the drug was safe and well-tolerated.
Significantly, the study also demonstrated a slowing in the atrophy (shrinking) of the caudate, a key part of the brain dramatically affected in HD, leading to a decline in cognition, function, and movement, Dr. Atkins said. Such atrophy occurs before symptoms appear, she noted, so being able to observe this change early makes the atrophy a good measure of a drug’s effectiveness.
The slower shrinking “was the first time this was shown in the clinic,” Dr. Atkins said. “We were super-excited to see this.”
With these promising results, Wave plans to put WVE-003 into a combined Phase 2/3 clinical trial, Dr. Atkins said. The company later this year expects to seek FDA approval of the trial. Wave proposes to use caudate atrophy as a primary endpoint, that is, a main measure of WVE-003’s effectiveness.
Wave is also investigating WVE-003’s potential impact on somatic expansion, Dr. Atkins said. Somatic expansion is the tendency of the mutant huntingtin gene to continue expanding over time. Many scientists now believe that this process triggers HD symptoms.
Somatic expansion is understood as a two-step process where expansion of the gene (step 1) triggers disease (step 2) that drives HD. Wave believes that lowering the bad protein selectively (with WVE-003) is likely to address the second step.
As with tominersen, WVE-003 is administered via a spinal tap. Votoplam is a pill.
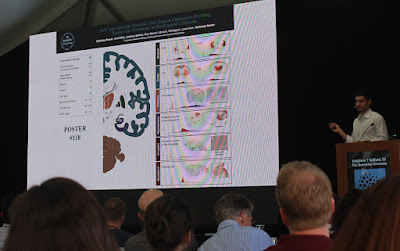
Dr. Jane Atkins of Wave Life Sciences displays a slide demonstrating the slowing of caudate atrophy in the WVE-003 clinical trial (photo by Gene Veritas, aka Kenneth P. Serbin).
uniQure drug slows disease progression in trial
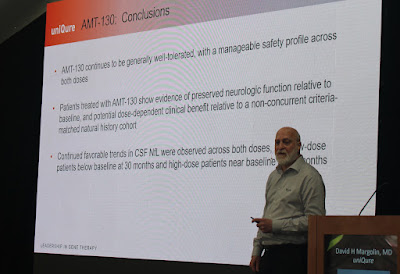
David Margolin, M.D., Ph.D., uniQure’s vice president for clinical development, gave a presentation on the latest developments regarding AMT-130, the firm’s gene therapy drug that reduces the levels of both the good and bad huntingtin protein.
In the uniQure clinical trial, a neurosurgeon injects AMT-130 directly into the brains of the volunteers under the guidance of an MRI. As a gene therapy, AMT-130 requires just this one application. (Watch the uniQure video about how AMT-130 is administered here).
This small, long-term uniQure Phase 1/2 trial began in 2020. As of April, the number of participants had reached 45, including people from the U.S. and Europe.
An interim analysis in mid-2024 showed that “AMT-130 high dose … strongly and significantly reduced disease progression,” Dr. Margolin pointed out. Another analysis found “substantial reduction in risk of clinically meaningful worsening,” he added.
As patients continue to go through the trial and beyond, with follow-up, “with every data cut we see… a promising treatment effect becoming more and more evident,” Dr. Margolin said.
Dr. David Margolin of uniQure presents data illustrating the slowing of HD disease progression in the AMT-130 clinical trial (photo by Gene Veritas).
Hoping to accelerate approval
The positive results have led uniQure to seek acceleration of FDA approval for AMT-130.
Because of HD’s status as a rare disease, in 2017 uniQure received the financially beneficial orphan drug designation from the FDA for AMT-130. In 2019, FDA granted AMT-130 fast track status to further facilitate development of the drug and expedite review.
As explained by Dr. Margolin at the conference, in 2024 the FDA defined AMT-130 as a regenerative medicine advanced therapy (RMAT).
This category includes life-threatening diseases such as HD. Dr. Margolin said it is applicable to new kinds of drugs such as gene therapy, cell therapy, and tissue-engineered products, and it further accelerates FDA review.
In achieving this designation, uniQure presented to the FDA the data from the Phase 1/2 trial, and the FDA agreed that this data can serve as the primary basis for a drug application, Dr. Margolin said.
Dr. Margolin indicated that this determination means that uniQure will not need to put AMT-130 into a Phase 3 trial.
“An additional investigational study will not be required,” he emphasized. “That accelerates by several years the timeframe in which AMT-130 might become available to a wider U.S. cohort of patients.”
Swaying the FDA to be more flexible
Because of the lack of therapies that modify the course of this rare and devastating disease, the uniQure project and the company’s dialogue with the FDA have indicated the willingness of the agency to allow flexibility in clinical trial programs and a faster timeline.
Dr. Margolin’s talk title included the phrase “alignment on a US Regulatory Path Via RMAT.” Alignment with the FDA could lead to an “accelerated approval” for AMT-130, he observed.
Dr. Margolin asserted that uniQure’s dialogue with the FDA “has meaningfully advanced HD regulatory science.”
In response to a question from Dr. Pacifici about the negotiations with the FDA, Dr. Margolin stated that uniQure hopes that the lack of disease-modifying therapy is “swaying FDA to be more liberal than they have been in the past.”
Dr. Pacifici asked what additional studies uniQure will conduct if it secures the accelerated approval, which would still be only conditional.
Dr. Margolin replied that uniQure will discuss that matter with the FDA.“Importantly, even an accelerated approval means the drug will be available to patients,” Dr. Margolin stressed. “It does constrain promotional materials in certain ways, but would have no relevant impact on its potential availability and accessibility to U.S. patients.”
A Breakthrough Therapy designation
AMT-130 gained RMAT designation because it is a gene therapy. Since the conference, the AMT-130 program has made yet further progress.
On April 17, uniQure announced that the FDA granted Breakthrough Therapy designation to AMT-130.
“Receiving Breakthrough Therapy designation underscores both the urgent need for effective treatments for Huntington’s disease and the encouraging interim data demonstrating that AMT-130 has the potential to slow disease progression,” said Walid Abi-Saab, M.D., chief medical officer of uniQure, in a press release. “We look forward to working closely with the agency to bring AMT-130 to the Huntington’s disease patient community as quickly as possible.”
As explained in the press release, Breakthrough Therapy
designation for AMT-130 means that the drug “may demonstrate substantial
improvement over available therapy on a clinically significant endpoint(s).”
The firm expects to provide a further FDA update this quarter. In the third quarter, it aims to present data on AMT-130 to support its potential drug application submission.