At the recent 20th Huntington’s Disease Therapeutics Conference, four companies provided updates on their key clinical trial programs, demonstrating that they had overcome basic safety hurdles and revealing plans to have their drugs potentially approved as therapies (treatments) for delaying the progression of HD symptoms.
PTC Therapeutics, Roche, Wave Life Sciences, and uniQure made 15-minute presentations. This clinical trials update took place during the first session on February 25, the first day of the three-day event.
Sponsored by the nonprofit CHDI Foundation, Inc., the largest private funder of HD research, the conference took place in Palm Springs, CA.
Possible impact
All four programs use drugs to lower the amount of harmful mutant huntingtin protein in the brain cells of patients. Blocking the bad protein could help prevent the death of brain cells, a major driver of HD.
In a post-conference interview with me, CHDI Chief Scientific Officer Robert Pacifici, Ph.D., said that the companies’ plans to move their programs towards drug approval is “great news.”
“All of them expressed their commitment to moving forward with their interventions, and that’s not trivial,” Dr. Pacifici said. “That means a lot of time, a lot of money invested on their part. They wouldn’t be doing it if they didn’t think there was great promise there.”
Each firm has overcome the basic safety hurdles necessary for moving to a Phase 3 clinical trial, the final step before the U.S. Food and Drug Administration (FDA) approves a drug, Dr. Pacifici added.
This article, the first of two, focuses on trials from PTC and Wave. Part II will examine the Wave and uniQure updates.
Votoplam, a potential pill for HD
With 60 companies represented at the conference, CHDI selected those “that had something new to say” in terms of clinical development, Dr. Pacifici told the attendees.
Amy-Lee Bredlau, M.D., PTC’s senior medical director, began her talk on the company’s huntingtin-lowering drug by noting progress: the compound, PTC518, is now called votoplam, a nonproprietary drug name assigned by PTC’s new, larger partner on the project, the international pharmaceutical firm Novartis.
“I think this is a really great collaboration,” Dr. Bredlau said.
As Dr. Bredlau explained, votoplam is a huntingtin splicing modulator, reducing the production of both the mutant and normal huntingtin proteins.
In contrast with riskier delivery methods, some presented in the session, votoplam is a pill. That makes it easy for patients to take the drug.
CHDI and PTC started the search for a huntingtin-lowering pill with a joint project initiated in 2018.
A delay in HD progression
PTC ran a successful Phase 1 clinical trial of votoplam in 2020 and 2021, providing initial evidence of safety and the lowering of the huntingtin protein.
At the conference, in an interim analysis, Dr. Bredlau presented data from the first 32 of the 156 volunteers enrolled in PIVOT-HD, PTC’s one-year global Phase 2 trial, which has verified the safety and tolerability of the substance. The first group of participants in PIVOT-HD began in 2022.
PIVOT-HD demonstrated that, by the third month, votoplam enters trial volunteers’ brains and lowers the huntingtin protein, she said. At month 12, the lowering was sustained. The trial also showed no spikes in neurofilament light chain (Nfl), a protein whose presence indicates degeneration of brain cells in diseases like HD. Scientists hope that lowering huntingtin will limit Nfl.
Significantly, Dr. Bredlau observed that these volunteers had a delay in the progression of HD symptoms, as indicated by several key clinical measures.
She said PTC is “very excited” about those trends, which “look very promising,” adding that “we’re really hopeful that we’ll see a strengthening of the signal at the end of the 12-month study,” when results from the remaining volunteers will be studied.
PTC will release full results of PIVOT-HD in this (second) quarter of 2025, said Dr. Bredlau, adding that the firm hopes that the results secure permission for a Phase 3 trial, to be run by Novartis.
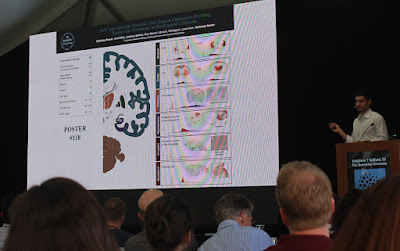
Dr. Amy-Lee Bredlau of PTC Therapeutics presents data from the PIVOT-HD clinical trial demonstrating trends of a delay in progression of Huntington's disease symptoms (photo by Gene Veritas, aka Kenneth P. Serbin).
GENERATION HD2 fully in progress
Peter McColgan, M.D, Ph.D., global development leader for Roche, updated the pharmaceutical giant’s HD program. He focused on the Phase 2 trial of the huntingtin-lowering drug tominersen.
Tominersen is an antisense oligonucleotide – a “laser-guided missile” against HD – originally developed by Ionis Pharmaceuticals, Inc. Like votoplam, tominersen lowers both the normal and mutant huntingtin protein.
After Roche’s unsuccessful trial of tominersen in 2021, the company redesigned a less ambitious and more focused trial of the drug in people less affected by the disease. Called GENERATION HD2, it started in early 2023.
Dr. McColgan reported that GENERATION HD2, by January, had fully recruited its target of 301 volunteers at 70 sites in 15 countries.
“This is a massive achievement,” he said.
The trial will assess tominersen’s safety, the use of biomarkers (signs of a disease and a medication’s efficacy), and the drug’s effectiveness.
Tominersen is not a pill. It is administered via a spinal tap.
Roche aims to complete the trial by the end of 2026.
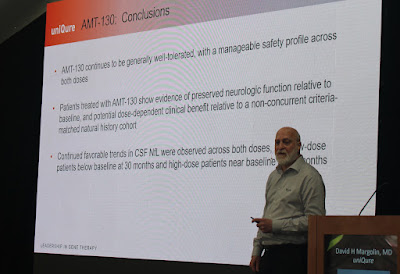
Dr. Peter McColgan of Roche with a slide showing the global recruitment for the GENERATION HD2 clinical trial (photo by Gene Veritas)
Roche’s multiple approaches
Dr. McColgan also described how Roche has expanded its focus to include other possible HD treatments and related research.
“We believe the fastest way to get treatments to patients is to pursue multiple programs in parallel,” Dr. McColgan said.
In collaboration with its colleagues at Spark Therapeutics – acquired by Roche in 2019 – Roche scientists are exploring other potential molecules for targeting HD. Spark specializes in gene therapies.
HD researchers continue to weigh the approach of drugs such as votoplam and tominersen, which lower both the mutant and normal huntingtin protein, versus those that attack only the mutant. The latter types are known as allele-selective. They leave the normal protein to carry out its essential actions unhampered.
Dr. McColgan said that Roche and Ionis are investigating an allele-selective antisense oligonucleotide.
Roche is also participating in the HD Regulatory Science Consortium. Using data from the original tominersen trial and other patient data, this collaboration seeks to improve the measurement of clinical trial volunteers’ performance in clinical trials, said Dr. McColgan.
Roche is also collaborating with CHDI to improve the measurement of Nfl (neurofilament light chain) as a key biomarker.
“Nfl increases across the stages of HD,” Dr. McColgan observed.
The latest news on tominersen
All clinical trials are regularly checked by an independent data monitoring committee.
Volunteers in the tominersen trial not on placebo have received either 60mg or 100mg of the drug.
On April 17 Roche issued a letter to the HD community stating that the committee overseeing the tominersen trial has found “no concerns … regarding participant safety or signs of symptom worsening with either tominersen dose.”
In addition, the letter said, “the 100mg dose was found to be more likely than the 60mg dose to result in clinical benefit. Therefore for the remainder of the study only the 100mg dose will be tested against placebo, and the 60mg dose will be discontinued.” Those receiving 60mg will now get 100mg.
“We are incredibly grateful to the 301 participants and their companions enrolled in GENERATION HD2,” the letter stated. “Each study visit contributes to collecting data that helps the entire HD research community learn more about tominersen, Huntingtin-lowering strategies, and the further understanding of HD.”
In Part II of this article I will report on Wave’s and uniQure’s clinical trial updates
(Disclosure: I hold a symbolic amount of Ionis shares.)