Pharmaceutical giant Roche’s historic gene-silencing clinical trial for Huntington’s disease is now ramping up, with the firm’s scientists “actively thinking” about when and how to expand research to target groups beyond the current criterion of early- to mid-stage HD patients aged 25-65, said the program’s scientific coordinator.
“We’re excited to be moving forward with the Phase 3 program,” said Scott Schobel, M.D., M.S., Roche’s associate group medical director and clinical science leader for the HD drug RG6042. He spoke in a February 26 interview with me during the 14th Annual HD Therapeutics Conference in Palm Springs, CA.
In the Phase 3 clinical trial, called GENERATION HD1, some groups are excluded, such as presymptomatic gene carriers like me (also known as prodromal or premanifest individuals) and juvenile Huntington’s disease (JHD) sufferers, because of the need to first prove RG6042’s efficacy in people where measurements can best be made and, in Dr. Schobel’s words, “most likely to show an effect.”
“Though we do not have a planned prodromal trial, we are actively thinking about what that would look like, should the lead studies be supportive of pursuing that route,” Dr. Schobel said. Similarly, for expanding to JHD and other age groups, “we’re also having discussions.”
“That desire [to expand access] comes from a place of having seen and interacted a lot with the community and understanding the severe unmet need of [treating] juvenile HD, on the one hand, and also the highly compelling nature of preventing the decline from occurring in the first place, the ultimate goal of a Huntington’s therapy,” Dr. Schobel explained. “Symptom reduction is great, and we hope to have great effects in manifest, but well recognize that the ultimate goal would be to help, let’s say, the ‘generation next’ that’s coming.”
At the moment, demonstrating RG6042’s effectiveness in GENERATION HD1 is Roche’s main goal. “For us to get to that expand strategy, we need to have confidence in evidence generation from the lead studies,” Dr. Schobel said. “I don’t think we’re there today, but I think we could hopefully get there in the course of the program.”
(The failure to discover effective Alzheimer’s disease treatments after hundreds of clinical trials has led researchers in that field to start including prodromal individuals in trials.)
Background on GENERATION HD1
Designed and tested in a successful Phase 1/2a clinical trial by Ionis Pharmaceuticals, Inc., RG6042 substantially lowered the amount of mutant huntingtin protein in the trial volunteers’ cerebrospinal fluid (CSF). Those impressive results prompted Roche, the drug’s license-holder, to accelerate the development of RG6042 and go directly to Phase 3.
In January, Roche announced that it had enrolled its first participant in GENERATION HD1. The trial is currently under way in Canada and the U.S., and Roche recently announced planned sites in Spain and the United Kingdom. It plans a total of approximately 660 participants at 80 to 90 sites in about 15 countries.
In addition to GENERATION HD1, all 46 participants in the Phase 1/2a study enrolled in a 15-month “open-label extension” (OLE) study that assesses the safety and tolerability of longer use of RG6042 and provides further data in support of GENERATION HD1. Those who got the placebo originally now get the medicine.
Roche is also conducting a 15-month observational study – without a drug – called The HD Natural History Study (NHS). It is gauging the natural progression of the disease in up to 100 participants with early-stage HD in Canada, Germany, the United Kingdom, and the U.S. This study seeks to deepen understanding of the role of the mutant huntingtin protein in the progression of HD.
RG6042 is a drug molecule known as an antisense oligonucleotide (ASO), an artificial strand of DNA. This particular ASO partially blocks the production of the huntingtin protein, the mutant form of which causes HD. RG6042 is a non-allele-specific ASO: it reduces, or lowers, both the mutant and normal (wild type) huntingtin protein. Researchers in other labs are working with allele-specific approaches to target only the defective huntingtin protein.
As in the Ionis trial, in GENERATION HD1 doctors inject the ASO into the CSF with a spinal tap (also called a lumbar puncture) into the so-called intrathecal space of the spine. Participants are receiving a monthly spinal tap over 25 months as part of a three-arm study (two with drug and one with placebo).
For details and background on GENERATION HD1 and the associated studies, click here, here, and here.
In late February, it was reported that Roche had agreed to pay $4.8 billion to acquire Spark Therapeutics, Inc., a Philadelphia-based biotech firm focusing on gene therapy approaches to genetic diseases, including HD. The potential significance of this pending deal is part of the discussion below.
Designing and executing the clinical trial program
Dr. Schobel, based at Roche’s headquarters in Basel, Switzerland, received his medical degree from the University of North Carolina at Chapel Hill. From 2001-2012, he was affiliated with Columbia University in New York City. He interned in medicine and neurology, did a residency in psychiatry, and was an assistant professor in both medicine and clinical psychiatry.
In 2013, the year Ionis and Roche agreed on a partnership, Dr. Schobel joined Roche as a translational medicine leader - focusing on the discovery of potential treatments to go into clinical trials.
In December 2017, he became the associate medical group director and full-time clinical science leader for the RG6042 program. He oversees the scientific design and execution of GENERATION HD1 and the associated studies, including the selection of the target population, the length, dosing frequency and levels, clinical outcome measures, and selection and assessment of biomarkers (signs of a disease or a medicine’s effect on it).
Dr. Schobel’s team collaborates with Roche data scientists on the system of digital biomarkers. He is also supporting the regulatory efforts for seeking health authority approvals for the clinical studies to run in the various countries involved in the study. His team also addresses any adverse events (AEs) that clinical trial volunteers might experience in the program.
“Really in this field at this time, this is absolutely a dream job,” Dr. Schobel said. “I wake up every day with utter enthusiasm for the potential of this molecule and to make sure that we do the best by seeing if it works or not, because we still don’t know.”
At the HD Therapeutics conference, sponsored by CHDI Foundation, Inc., Dr. Schobel was the senior author of the scientific poster that won third place in a competition that involved a record 115 posters. The poster resulted from research based on electroencephalography (EEG) readings of brain waves taken from the participants in the Phase 1/2a trial.
The work confirmed the EEG readings as potential biomarkers for clinical studies. (Click here to watch a presentation of the poster by Lauren Boak, Ph.D., of Roche. For further background on EEG, click here.)
Just before our interview, Dr. Schobel participated in a CHDI panel discussion on the question: how should the HD community prepare to follow up on the results of the huntingtin-lowering clinical trials, whether positive or negative? We addressed that and other key themes.
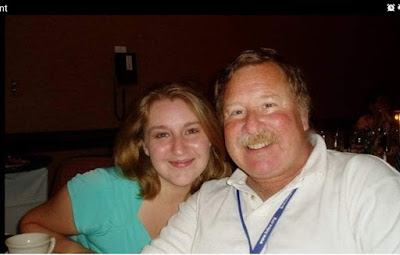
Scott Schobel, Ph.D., M.S., of Roche, with Anne Smith, Ph.D., Ionis director of clinical development, at the 2019 HD Therapeutics Conference (photo by Gene Veritas)
Several years to complete the study
GV: How many participants have enrolled so far in GENERATION HD1?
I can say that there are several sites open already in the U.S., Canada, and, as we just announced, we’re imminently starting up in the United Kingdom and Spain. We’re essentially in a ramping up phase of the pivotal study.
I think we’ve had a good start, though. We've met our target to enroll either by the end of 2018 or early 2019. That’s a massive accomplishment, from only one year ago completing Phase 1. We’re happy and proud about that.
GV: For each participant, it’s a 25-month study. Can you project at this point how long the trial will last?
SS: We don’t know exactly at this point. If you assume that recruitment’s not going to happen overnight, and we have a two-year treatment length, then we have to plan on it being at least a few years for the primary outcome from the trial [to be ascertained]. It’s always based on when that last person is enrolled.
We think that [the 25-month study] length is necessary. We don’t want to sell short the ability to judge drug effect. It may take some time to determine adequately benefit/risk ratio.
Considering the broad continuum of HD
GV: The CHDI panel in which you participated today (February 26) asked how the HD community should prepare for both positive and negative trial results. What is the takeaway message?
I think there was a call for collaboration for leveraging the strength of the biological pathway [lowering the huntingtin protein] to enable more rapid assessment whether drugs are effective or not. I think there was a focus on being sensitive to covering the [various] stages of disease with the interventions [treatments] and not just focus narrowly on one stage of disease, but try to broaden that out, to de-risk the possibility that therapies may be more or less effective along [certain points of] the continuum of HD.
I was very thankful actually that CHDI organized that, because I think that getting us as a community, including industry but also academics and the broader community, to start thinking of these questions together proactively is a really good thing.
GV: The trial drug is for people aged 25 to 65. If the drug is successful and approved, would that mean that only people between 25 and 65 could take the drug? Would it specify that range on the label? Or would it be something that doctors could prescribe as they saw fit?
SS: This is a complex question, because it involves what regulators do when they grant a label, depending on study results. But we should not speculate.
Despite a scenario of regulatory approval, there’s still the issue of access to the medicine. For access, as I’ve learned from my colleagues who are focused on this area, this is about the evidence package in support of giving the medicine to a population who you know will benefit based upon the evidence.
We wanted to start with a target population we knew would be sensitive to decline over the observation period, so that if our drug works we can measure the effect.
The studies are designed to provide health authorities with the required data so that the benefit-risk of RG6042 can be determined as quickly as possible. The ultimate goal is that RG6042 can be approved by health authorities and made accessible to the broader HD community.
Because that’s our primary purpose: if we don’t set ourselves up for success on our trial, none of those issues will ever matter, because you haven’t even proved the main point in the population most likely to show an effect, in our best judgment. A little narrow by design, but with the ambition to go broader, with more evidence generation.
Building the evidence for RG6042
GV: What is your scientific assessment of RG6042 as a potential HD drug?
SS: I feel very good about the potential of RG6042,but there is more we need to learn to fully understand the benefits and risks of RG6042. I’m well aware of a truly exhaustive preclinical set of studies [in animals], which optimized this particular molecule for clinical development. That was done head-to-head versus allele-specific agents, other non-allele-specific ASO agents, and this candidate essentially proved that it was efficacious across multiple models and also safe and tolerated, including what is now a completed toxicology package, including a chronic nine-month study [the Phase 1/2a study, which involved four doses over three months, plus six months of observation]. I’m very confident that we have a good molecule in the clinic on that basis.
What’s now better still is that we’ve had our successful completion of the Phase 1/2a study. Though I can’t comment specifically on aspects of the ongoing OLE, because that will only be presented in organized forums like podium presentations, etc., I can say now that we’ve been in that study over a year, so that also gives me confidence that this is something that could be suitable for a chronic treatment paradigm.
I think the pieces that need to come in now are the things that are going to take a little longer, that might require some patience, importantly efficacy and long-term safety in a larger group of patients. We’ll await the randomized [Phase 3] trial result, as the ultimate confirmation of that.
The open-label extension is our most advanced study. We’re quite focused on learning about the drug from that study, comparing the two treatment regimens [different frequency of drug] and the associated safety/tolerability, PK of the drug [pharmacokinetics: absorption, distribution, and metabolism of a drug], PD [pharmacodynamics: effect and mechanism of a drug] and exploratory clinical outcomes over 15 months, although note this is in an open label/not placebo-controlled setting. That’s obviously going to finish before the end of the pivotal study.
We’re pairing that with a Natural History Study to understand what we can be most confident of measuring in the open-label study, which is measures on objective biomarkers like mutant huntingtin. We can compare that against this matched natural history cohort over a longer time frame to understand not only the longer term safety/tolerability from the OLE, but also then the putative efficacy on the biomarkers and the clinical outcomes and digital clinical outcomes that are in the OLE study.
We’re in a very good spot and moving forward.
Expanding access to other disease groups
GV: So, the people in OLE will stop at 15 months?
SS: No. There is another study, which actually has been drafted and planned, that is essentially an extension of the first OLE study. And that’s known as the GEN-EXTEND Study. That will be an extension study for all participants of Roche- or Genentech-sponsored studies: the OLE, NHS, and GENERATION HD1.
[In the U.S., Roche personnel and products still use the name Genentech, a major U.S.-based biotech firm acquired by Roche in 2009.]
GV: Let’s say GENERATION HD1 takes four years. So, the people from Phase 1 through GEN-EXTEND will be able to continue that entire time?
SS: Yes, that’s right – if they wish. We’re not going to leave anybody who’s been committing their precious time to be in a Roche study to not continue treatment while they wait.
GV: When you say “expand,” which you referred to at the CHDI panel, you’re thinking about including prodromal individuals at some point?
SS: Exactly. We need to get information from the lead studies in manifest HD first. Though we do not have a planned prodromal trial, we are actively thinking about what that would look like, should the lead studies be supportive of pursuing that route. We have a strategic mindset, and we indeed want to fully test the lowering hypothesis. And we fully believe that HD is a spectrum, so those planning discussions are consistent with that philosophy.
There are other aspects. As a part of drug development requirements, in the European Medicines Agency [the equivalent of the U.S. Food and Drug Administration] you’re required to come up with a pediatric investigational plan in juvenile HD, which we care about greatly as well.
That desire comes from a place of having seen and interacted a lot with the community and understanding the severe unmet need of [treating] juvenile HD on the one hand and also the highly compelling nature of preventing the decline from occurring in the first place, the ultimate goal of a Huntington’s therapy. Symptom reduction is great, and we hope to have great effects in manifest, but well recognize that the ultimate goal would be to help, let’s say, the “generation next” that’s coming.
Gaining confidence in the drug
GV: Since the confirmation of Phase 3 at the 2018 CHDI meeting, what new insights have you gained about the drug and HD, including from the open-label extension of Phase 1/2a? Can you elaborate on anything beyond what we’ve already discussed?
SS: I can just say that, broadly speaking, we’re very happy to be in the position where we have an open-label extension study that’s generating information on a regular basis. That gives us more confidence in the chronic therapy paradigm. We weren’t there a year ago. We just had had a four-dose study. Now we’ve had an OLE study running over a year. Further details from that will need to await our organized planned presentations, but we fully intend to share on that experience as this year progresses. The details of that are pending an ongoing set of analyses that we have.
GV: Have there been any adverse events in the OLE?
SS: Well, every drug program has AEs. There are nuances and details of what kinds of AEs. I’m just not at liberty to talk about those at this time, mainly because we don’t have the analysis on our full data set and we will be presenting at a later date during the course of the year.
GV: But if something severe happened, you’d have to stop.
SS: Exactly. A really critical aspect of that is that we’re required by regulatory authorities to give any update of new safety signals, and we do that, if it comes up. Similarly, we have regular feedback from our network of investigators. So, it’s this sort of constant triad of communication that we do. We’re watching this with a magnifying glass.
GV: Are there any new findings that you can report regarding biomarkers?
SS: Clearly this is of high interest to everyone. We fully intend to communicate this type of information as it becomes available and as the program matures. I think we’re well-positioned with this drug to anticipate more biomarker findings.
The Spark acquisition and broadening the drug playing field
GV: What does Roche’s pending acquisition of Spark Therapeutics mean for GENERATION HD1?
SS: Just a disclaimer: I’m not allowed to speak of any details. The short answer is: absolutely no effect on GENERATION HD1. We’re fully committed to developing this ASO, RG6042.
GV: I meant in a positive sense, not that it’s going to interrupt GENERATION HD1. But, with Spark’s knowledge and technology entering into the mix, what other possibilities does it open up for Roche in terms of tackling HD?
SS: I think it does, broadly speaking, open up possibilities. I think it’s premature, even for our program, to give a specific answer about how that might take shape other than to give the general message that it’s a positive. Broadening the playing field of therapeutic options that lower huntingtin is a good thing. I think that should be rightfully recognized by the HD community as well.
GV: They and other people work with viruses to deliver drugs. Is there any way RG6042 could be delivered via a virus?
SS: I don’t know the answer to that question. ASOs don’t need vectors, because basically they freely diffuse into cells and tissues. I don’t know that you’d even want to go to the trouble of putting it into a virus. As long as you’re getting an ASO into the CNS [central nervous system], to the intrathecal space, that in principle could be up high through the ventricles [the center of the brain] or anywhere along the neural axis [CNS]. It’s never come up as a strategic priority or focus.
What we are focused on is exploring alternate modes of delivery for the ASO. We like the idea that ASO therapy generally is periodic, dose titratable [adjustable], reversible. The thing we hope to do over time is to be able to learn and optimize a frequency of administration and dose of administration, to limit the burden of repeated lumbar punctures. Maybe through a device you don’t have to always access the intrathecal space. These are things we actually think about, because we well recognize that if this therapy works, it will be a chronic therapy.
Alternative drug delivery methods
GV: Is there any update you can give on brain shuttle research at Roche? As a technology that could get a drug past the blood-brain barrier, the brain shuttle might allow for a drug in the form of a pill.
SS: The brain shuttle technology is generally being pursued at Roche aggressively. It is not our lead strategy with this molecule, which is already having such promise through the intrathecal route. Could that still be a future possibility? I can’t really speculate on that, because it’s right now not in our core focus. What we need to do now with this ASO is test the hypothesis: does it work for HD? We know that that we can do that successfully with confidence through the intrathecal route. Once we do that, then we open up all kinds of possibilities for delivery modalities, including, in principle, technologies like the brain shuttle.
GV: You mentioned the word device. Would that be a pump?
SS: You must give ASOs by bolus injection [a single, large administration of a drug], generally. That promotes distribution. If there were a lumbar intrathecal device, it could help you access that bolus through a subcutaneous route and a port rather than needing to always go with the spinal needle into the intrathecal space. That kind of innovation is an example of what we’re actively thinking about.
I can say that the intrathecal procedure, having now been steeped in it – and I’ve done a lot of lumbar punctures in my past role as a medical doctor before joining Roche, I’ve never done intrathecal dosing, but I’ve seen a lot now, talked a lot, and we know how it’s going in our studies – this is essentially a 20-minute procedure that’s outpatient.
We collaborate very closely with our investigator network that does intrathecal. This is the big focus: to educate. I helped co-produce a video of best practice that we’re using in our investigator network. I think those are the kinds of efforts that we need to be doing as a community, to promote best practices and the ability to receive the drug, if it works.